
Revenue Intelligence Built for RCM
Turn insight into impact with real-time visibility and built in resolution paths that keep your RCM moving forward.
See How It Works


About Adonis Intelligence
Intelligence partners with revenue cycle teams to maximize recoverable revenue, boost AR velocity, and optimize billing workflows - all while saving time and reducing costs.


Unify RCM Data
See the full picture of your revenue cycle ecosystem
Stay Ahead
Keep up with ever-changing payer behaviors and compliance requirements
Maximize ROI
Drive team efficiency, increase speed to cash, and reduce days in AR

Identify Revenue Roadblocks Maximize Opportunities
Supercharge Your RCM Team with Intelligence
Combine the best of AI technology and RCM industry expertise.
Get strategic guidance and recommendations across:
- DENIALS
- collections
- accounts receivable
- productivity
- underpayments
- Overpayments
Track KPIs That Matter Most
High-level executive dashboards and detailed drill-down reports are accessible across all levels of your organization.
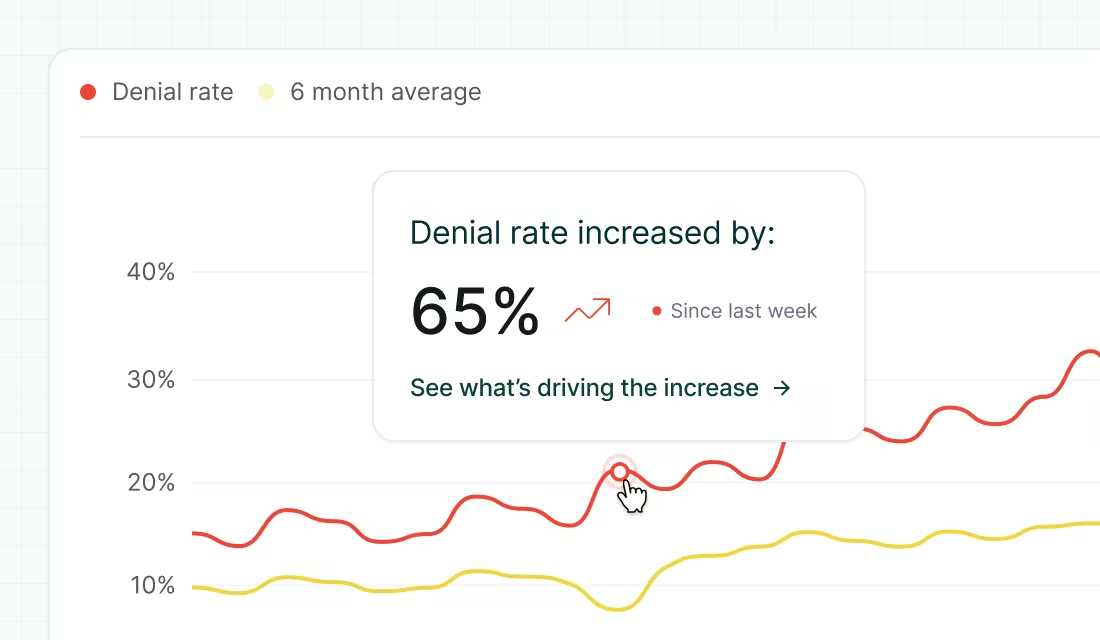
Uncover Gaps with AI-Powered Alerting
Diagnose revenue leakage and uncover hidden trends and opportunities across your end-to-end revenue cycle.

Find True Underpayments, Not False Flags
Prioritize and resolve underpayments efficiently to increase collections and prevent further revenue loss.
Accelerate Cash Flow with Smart Focus
Eliminate the guesswork and take immediate action on the claims with the greatest impact on your bottom line.












.svg)





.svg)







.svg)