Inside Momentum 2025: What Practices Are Saying About Denials, Payers, and Staff Strain
This November, our team had the pleasure of sponsoring a booth at ModMed Momentum 2025. Held in Orlando and drawing specialty practices from across the country, Momentum continues to be one of the most valuable forums for connecting with the providers and operators shaping the future of specialty care.
We were especially excited to attend this year as the industry continues to experience rapid change, driven by staffing shortages, rising payer pressure, and accelerating adoption of AI-powered solutions. Momentum 2025 reflected all of it through forward-looking product innovation, hands-on education, and candid peer discussions about what is really happening inside today’s practices.
What We Heard Across Specialties
Throughout the conference, we had the opportunity to speak with leaders and operators from a wide range of specialties, from dermatology and gastroenterology to orthopedics, ophthalmology, and beyond. While each specialty has its own nuances, one thing became abundantly clear: the revenue cycle challenges they face are remarkably consistent.
Across the board, practices shared a common frustration with the growing complexity of payer behavior. Policy changes, shifting rules, inconsistent interpretations, and opaque reimbursement decisions continue to make revenue cycle operations harder to predict and harder to manage.
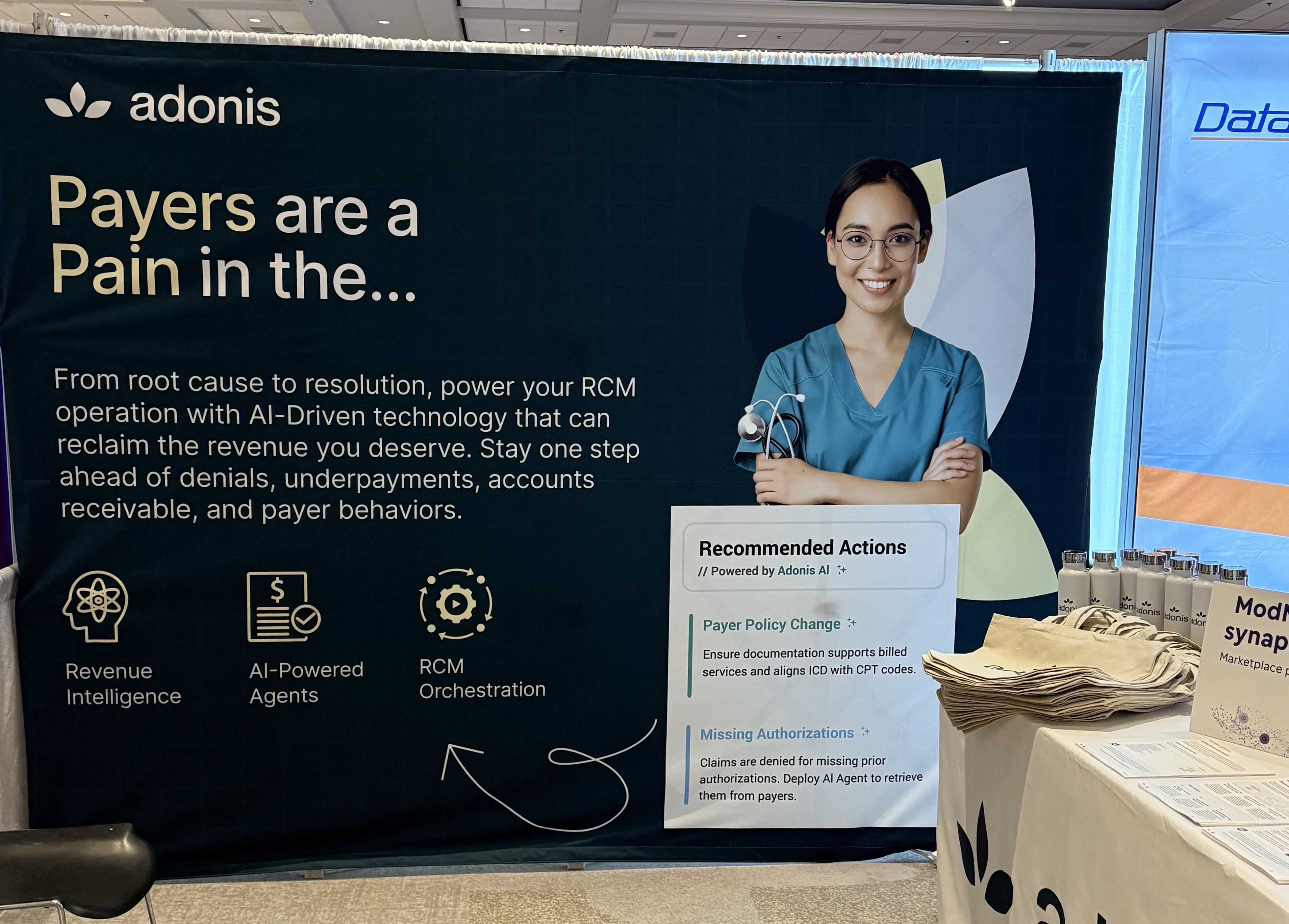
In more candid terms, many attendees echoed the same simple sentiment. Payers are a pain. And that pain is being felt most acutely in denials.
Denials Are Outpacing Teams
One of the most common threads we heard was how difficult it has become to keep pace with denials using small, stretched teams. Even highly experienced billing and AR staff are struggling to stay ahead of rising denial volumes, especially as medical necessity edits, prior authorization requirements, and retroactive policy changes become more aggressive.
Several practices told us that what used to be a manageable backlog can now spiral quickly. Denials sit too long. Appeals fall behind. Teams end up working reactively instead of strategically. And when that happens, cash flow suffers.
Making matters harder, many organizations simply do not have the option to add headcount. Between hiring challenges, budget constraints, and burnout risk, just hiring more people is no longer a viable solution for most practices.
The Push to Do More With What You Have
Because of this reality, one of the strongest themes we heard at Momentum was the urgent need to do more with existing teams. Practices are actively searching for ways to increase output, improve recovery, and reduce manual work without burning out their staff.
Leaders shared interest in:
- Automating manual denial workflows
- Prioritizing high-impact work instead of first in, first out queues
- Gaining better visibility into payer behavior and root causes
- Using data and AI to work smarter, not longer
There was clear openness to technology that can help teams scale their performance without sacrificing accuracy or compliance. At the same time, practices were thoughtful about adoption. They want solutions that integrate into workflows, not tools that create more work.
A Broader Shift Toward AI-Powered Operations
Momentum 2025 also made one thing clear. The industry is moving steadily toward an AI-powered future, not just in clinical documentation, but across front office and back office operations. From ambient documentation to smarter workflows and decision support, practices are increasingly expecting technology to actively assist, not just store information.
For revenue cycle leaders, this shift represents both opportunity and urgency. Those who modernize their operations now stand to gain significant advantages in speed to cash, staff productivity, and financial resilience.
Looking Ahead
Momentum 2025 reinforced something we see every day in our work. The revenue cycle is under more pressure than ever, but practices are ready for change. Despite staffing strain, payer friction, and operational complexity, there is real momentum toward smarter, more automated, and more resilient financial operations.
We left the conference inspired by the honesty of the conversations, the innovation on display, and the determination of specialty practices to adapt and thrive, even in the face of mounting challenges.
To everyone who stopped by our booth, shared their experiences, and engaged in meaningful dialogue, thank you. We are excited to continue these conversations and to keep working alongside you to build a more efficient, transparent, and sustainable revenue cycle.












